New projections and momentous FDA clearance of blood test highlight Alzheimer’s challenge
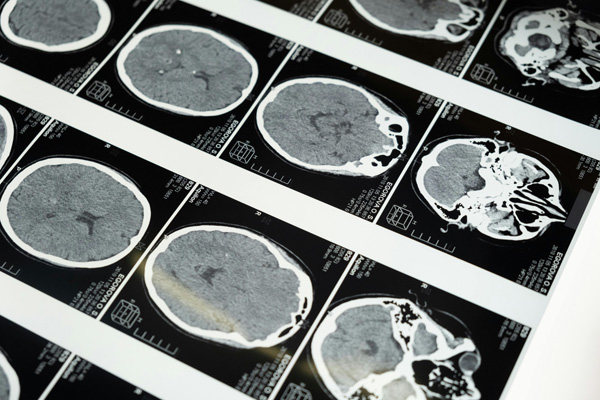
[Photo Credit to Pexels]
Biomedical researchers are urging immediate attention as a survey published in Nature Medicine earlier this year showed that 42 percent of Americans over 55 are projected to develop dementia in their lifetimes—and the FDA has just cleared the first blood test to help detect Alzheimer's disease more easily, representing both a critical healthcare and a significant advancement in cognitive care.
Dementia, a syndrome characterized by progressive declines in memory, reasoning, and daily functioning, has been on the rise persistently as life expectancy and quality have steadily increased.
Led by leading experts of the field, the landmark study revealed that more than 4 in 10 Americans aged 55-95 are expected to develop dementia sometime during their lives.
Notably, the risk found to be particularly elevated among women, Black adults, and carriers of the APOE4 gene variant.
Utilizing the estimations and the U.S. Census population projections, the study forecasts an alarming rise in annual new dementia cases: the 514,000 in 202 is expected to nearly double to 1 million by 2060.
The most substantial increase is expected among Black Americans.
These stark findings not only underscores the urgent need for public health strategies and structures that promote and support healthy aging, but also stresses the importance of addressing existing disparities in disease burden that further exacerbate the impact on high-risk populations.
In related development, recently this May 16th was a historical advancement in cognitive diagnosis and care: the U.S. Food and Drug Administration (FDA) granted clearance for the first blood-based diagnostic test for the disease.
Developed by Fujirebio Diagnostics, the Lumpipuls G pTau217/ß-Amyloid 1-42 Plasma Ratio measures two key proteins—pTau217 and β-amyloid 1-42—in blood plasma and yields a ratio linked to amyloid plaque,, a hallmark of Alzheimer’s disease pathology.
Clinical validation involving nearly 500 plasma samples of cognitively impaired adults, the accuracy of identification in presence of plaques came out to be 92%.
Neurologists note that the test represents a major step toward accessible diagnosis, far less invasive than PET scans or spinal taps.
The convenience of the tasks also make it highly deployable in primary care settings, making the step towards receiving help and further treatment easier.
These developmments—rising dementia risk and a new diagnostic tool for clinical use—come at a critical moment.
With cases projected to double over the next four decades, health systems may face extreme strain as the current system cannot support the sheer increase and unprecedented volume.
However, the FDA’s clearance signals progress: the outlook of an easier, faster diagnosis could forecast more, earlier interventions, improve patient planning and communication, and increase access.
Experts caution, however, that early diagnosis does not equate to a cure.
Although therapeutic options are available, they offer modest benefits and come with side effects.
Additionally, equity still remains a concern as projections illustrate a disproportionate increase in dementia, as well as other cognitive impairments, among underserved groups.
It is therefore imperative that institutions and government agencies invest in future developments that can further expand access, sustain prevention, and promote innovation.
Proactive and preventative action, supported and sustained by health policy and preventative strategies, will be essential in addressing these issues meaningfully.

- Jiwoo Bang / Grade 10
- The Madeira School

![THE HERALD STUDENT REPORTERS [US]](/assets/images/logo_student_us.png)
![THE HERALD STUDENT REPORTERS [Canada]](/assets/images/logo_student_ca.png)
